Outside of the brain, the heart is probably the organ that you miss the most when it ceases to function correctly. Unfortunately, as we cannot grow custom replacement hearts yet, we have to keep heart patients alive long enough for them to receive a donor heart. Yet despite the heart being essentially a blood pump, engineering even a short-term artificial replacement has been a struggle for many decades. A new contender has now arrived in the BiVACOR TAH (total artificial heart), which just had the first prototype implanted in a human patient.
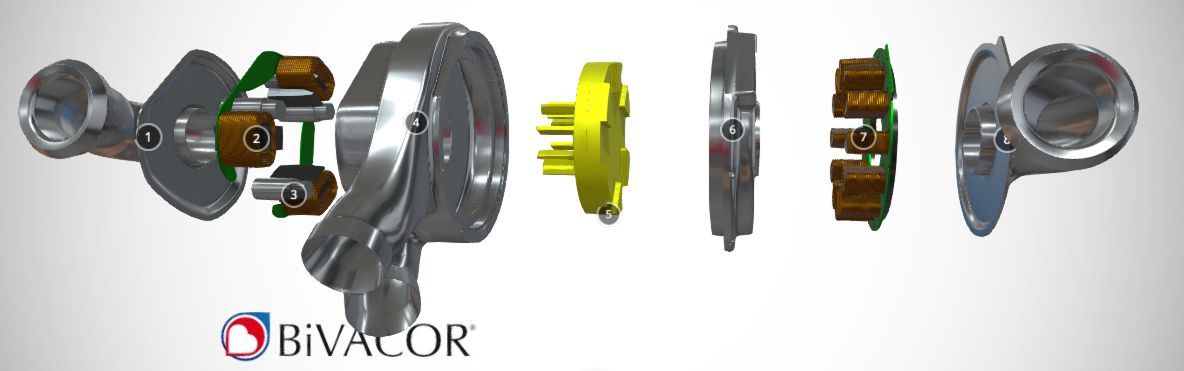
Unlike the typical membrane-based pumps, the BiVACOR TAH is a rotary pump that uses an impeller-based design with magnetic levitation replacing bearings and theoretically minimizing damage to the blood. This design should also mean a significant flowrate, enough even for an exercising adult. Naturally, this TAH is only being tested as a bridge-to-transplant solution, for patients with a failing heart who do not qualify for a ventricular assist device. This may give more heart patients a chance to that donor heart transplant, even if a TAH as a destination therapy could save so many more lives.
The harsh reality is that the number of donor hearts decreases each year while demand increases, leading to unconventional approaches like xenotransplantation using specially bred pigs as donor, as well as therapeutic cloning to grow a new heart from the patient’s own cells. Having a universal TAH that could be left in-place (destination therapy) for decades would offer a solid option next to the latter, but remains elusive. As shown by e.g. the lack of progress with a TAH like the ReinHeart despite a promising 2014 paper in a bovine model.
Hopefully before long we’ll figure out a reliable way to fix this ‘just a blood pump’ in our bodies, regardless of whether it’s a biological or mechanical solution.